Allergens at Growing Plates
Growing Plates was created by a medical doctor and mother who understands both the science and the emotional weight of feeding babies safely. Our goal is not just to nourish children, but to support parents with confidence, clarity and evidence-based care — without fear or overwhelm.
Introducing allergens can feel overwhelming — especially in the first year of life. Avoiding allergens without a medical reason does not prevent food allergy. In fact, evidence shows that early, appropriate exposure helps build tolerance.
Our meals are carefully designed to support this process safely, while giving parents clarity and confidence.
This page explains:
What each allergen is
How to introduce it safely (baby-appropriate forms)
What a reaction can look like
What to do if a reaction happens
When its an emergency (anaphylaxis)
FAQ’s
Important: This information supports (but doesn’t replace) care from your GP/allergist. If you suspect anaphylaxis, treat as an emergency and follow an action plan.
How we manage allergens at Growing Plates
We follow Royal Children’s Hospital (RCH) and Australasian Society of Clinical Immunology and Allergy (ASCIA) and Australian infant feeding guidelines, which support the early and safe introduction of common food allergens once babies are ready for solids
Introduce allergens around 6 months, not before 4 months) but within the first year of life, when developmentally appropriate
Prepared in safe textures to reduce choking risk
Clearly labelled on every meal
Designed for ongoing exposure once tolerated
Guided by Australian paediatric and allergy evidence
Evidence-based - Developmentally appropriate - Clearly labelled
What each allergen is (there is 9 of them!)
-

Cow’s Milk Protein
Cow’s milk protein allergy is one of the most common food allergies in infancy and is caused by an immune reaction to proteins in cow’s milk.
It is important to distinguish this from lactose intolerance, which is not immune-mediated and is rare in infants.
Symptoms may include eczema flares, hives, vomiting, diarrhoea, reflux-like symptoms, or blood or mucus in stools. Less commonly, respiratory symptoms can occur.
Cow’s milk can be introduced from around 6 months in age-appropriate forms such as yoghurt, cheese or milk cooked into foods.
Evidence suggests that early introduction may reduce the risk of allergy development.
Many children outgrow cow’s milk allergy during early childhood, but any suspected reaction should be medically assessed.
-

Wheat
Wheat allergy is distinct from coeliac disease and may cause hives, vomiting, abdominal pain or respiratory symptoms shortly after ingestion.
Wheat can be introduced in the first year of life once solids are established, commonly through wheat-based cereals, bread softened with liquid, or pasta prepared in soft textures.
Current evidence shows no benefit in delaying wheat introduction to prevent allergy.
-

Eggs
Egg allergy is common in babies and toddlers, particularly during the first year of life.
Egg contains several proteins that can trigger an immune response. Some children react only to lightly cooked egg, while tolerating egg baked into foods such as muffins or pancakes — because heat alters the protein structure.
Regular exposure to tolerated forms of egg is associated with improved tolerance over time.
Egg allergy is often temporary, with many children outgrowing it as their immune system matures.
-

Sesame
Sesame is an increasingly common cause of food allergy in Australia and is now recognised as a priority allergen.
Sesame is found in foods such as tahini, hummus, breads, crackers and baked goods.
Sesame should be introduced in infancy in small amounts, for example tahini mixed into purée or yoghurt.
Sesame allergy can cause severe reactions, including anaphylaxis, so any suspected reaction requires prompt medical assessment.
Regular inclusion is recommended once tolerated.
-

Peanut
Peanut allergy is one of the most significant food allergies due to its potential severity and persistence into adulthood.
Strong evidence shows that introducing peanut in infancy significantly reduces the risk of peanut allergy, including in higher-risk children.
Peanut should be introduced in the first year of life in a smooth, diluted form, such as smooth peanut butter mixed into purée, yoghurt or porridge.
Whole peanuts and thick spoonfuls of nut butter are choking hazards and should never be offered to infants.
Once peanut is tolerated, regular inclusion is important to maintain immune tolerance.
-

Tree Nuts
Tree nuts include almonds, cashews, walnuts, hazelnuts, pistachios and others.
Allergy may occur to one or multiple tree nuts, and tolerance to one does not guarantee tolerance to others.
Whole nuts are a significant choking risk and should not be offered to young children.
Tree nuts should be introduced as finely ground nut meal or smooth nut butter mixed into food.
Reactions can range from mild skin symptoms to anaphylaxis.
Early introduction in safe forms is encouraged, and ongoing exposure is important if tolerated.
-

Soy
Soy allergy is less common but may occur, particularly in children with other food allergies such as cow’s milk allergy.
Soy is found in foods like tofu, soy yoghurt, soy flour and many processed foods.
Soy can be introduced safely during infancy in age-appropriate forms such as mashed tofu or soy-based yoghurt.
Most children with soy allergy outgrow it during childhood, but reactions should be assessed by a healthcare professional.
-

Fish
Fish allergy can cause rapid reactions including hives, vomiting or breathing difficulties.
Fish should be introduced during the first year of life as well-cooked, deboned fish that is finely flaked or mashed into meals.
Early introduction may reduce allergy risk and provides important nutrients, including omega-3 fatty acids essential for brain development.
Unlike some other food allergies, fish allergy is less commonly outgrown and should be taken seriously.
-

Shellfish
Shellfish includes crustaceans (such as prawns, crab and lobster) and molluscs (such as scallops and mussels).
Shellfish allergy often develops later in childhood but can occur in infancy. Reactions can be significant and may persist into adulthood.
Shellfish should be introduced only when a child is developmentally ready, in well-cooked, finely chopped or mashed forms.
Initial exposure should be in small amounts with careful observation.

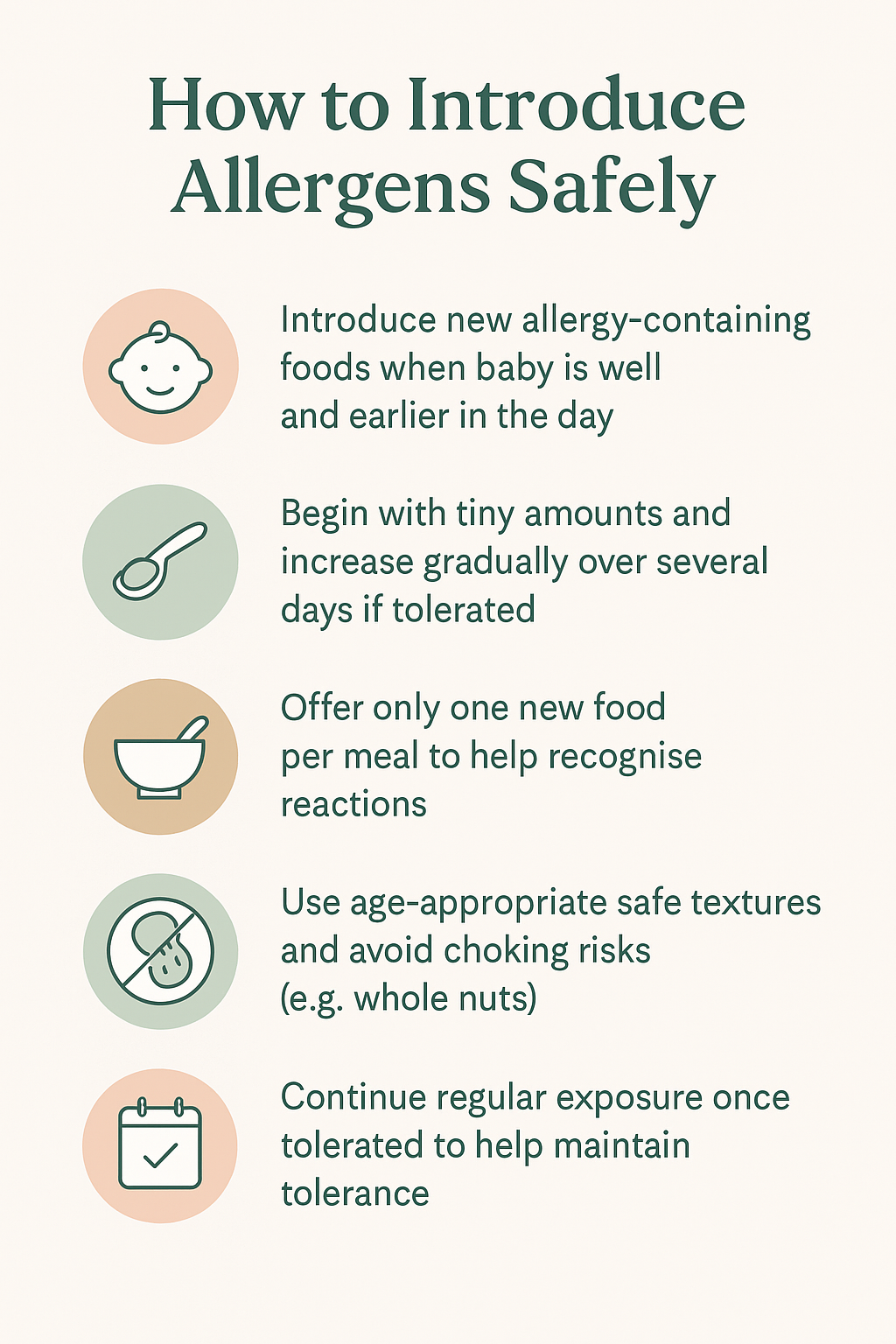
When your baby is ready for solid foods (typically around 6 months, but not before 4 months), begin introducing common allergenic foods in a methodical, stepwise way while they are well and you can observe them for a few hours afterwards.
Start with a very small amount of the new food (such as ⅛–¼ teaspoon) and gradually increase to a normal infant portion over several days if no reaction occurs.
Introduce only one new allergenic food at a time at a meal so that, if a reaction happens, the responsible food can be identified easily. It is best in the morning, before any other meals and can be closely observed throughout the day.
Use age-appropriate textures and safe forms — for example, smooth peanut paste or thinned smooth nut butter mixed into purée, well-cooked and finely mashed egg, or soft versions of wheat, soy, sesame and other allergens — and avoid whole nuts or large pieces that pose a choking risk.
Once an allergenic food has been introduced and tolerated, continue to include it regularly (about 2–3 times per week) as part of a varied diet to support ongoing immune tolerance; inconsistent or infrequent exposure can increase the chance of allergy development.
If any allergic reaction is suspected, stop the food immediately and seek medical advice before re-introducing it, and follow your baby’s ASCIA Action Plan if one has been provided.
Allergic reactions
-
How to spot an allergic reaction
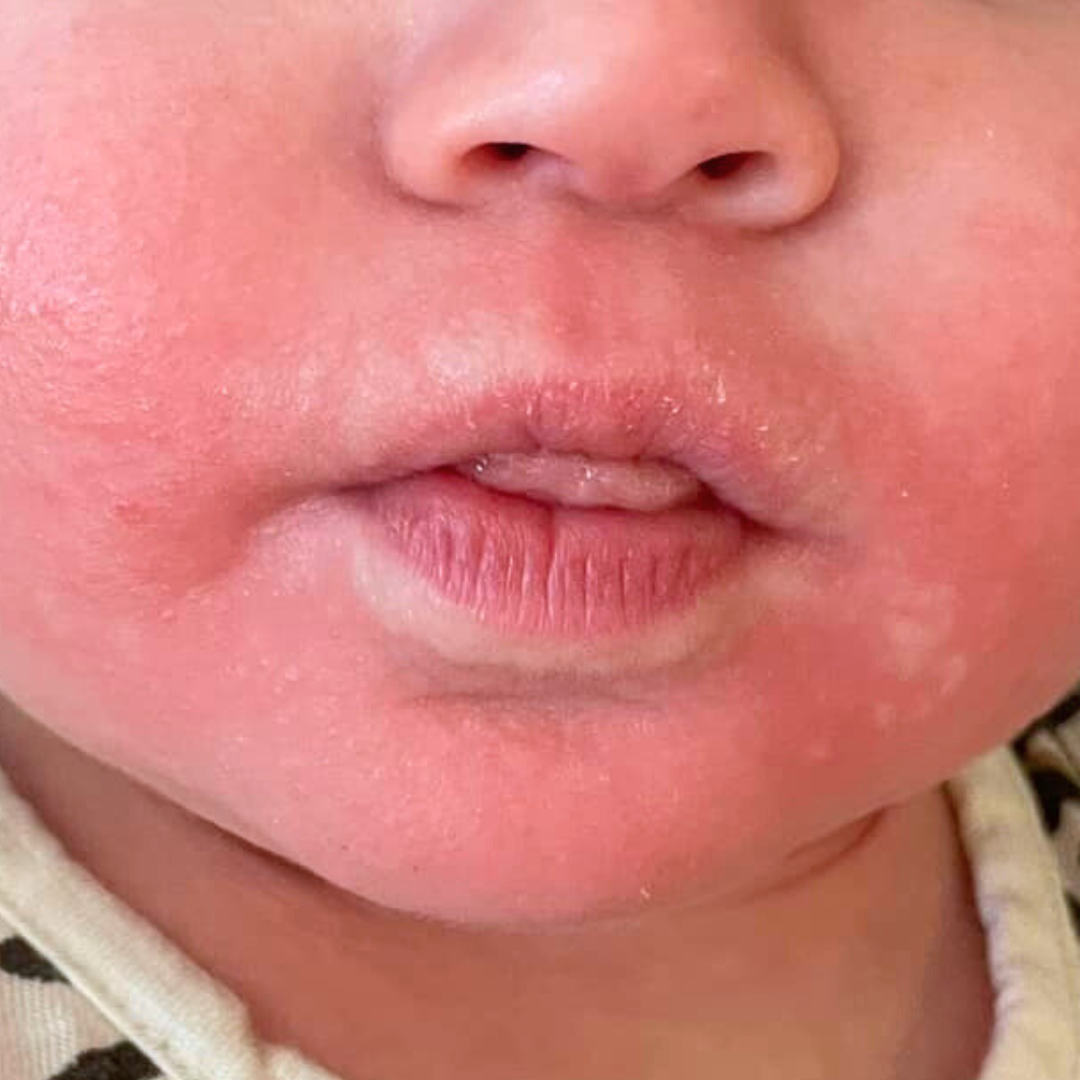
Allergic reactions usually occur within minutes to 2 hours after eating a food. Reactions can be mild, moderate or severe, and symptoms may involve the skin, gut or breathing.
Common signs of a mild to moderate reaction
Hives (raised, itchy red welts on the skin)
Redness or flushing of the face or body
Swelling of the lips, eyes or face
Vomiting
Abdominal discomfort or distress
These reactions can look alarming but are usually not life-threatening. However, symptoms can sometimes progress
-
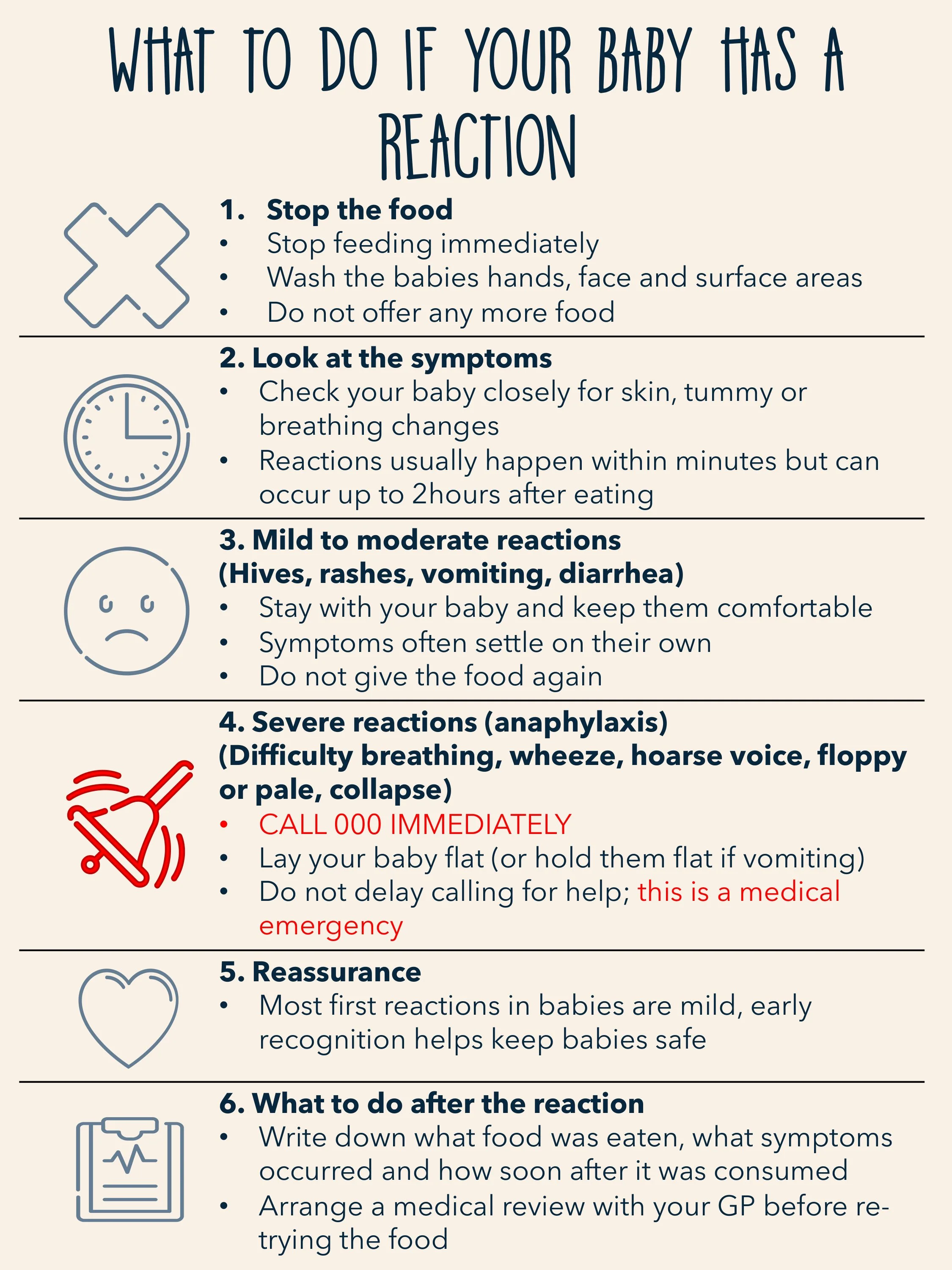
Stop the food immediately
Stay with your baby and observe closely
Do not offer the food again until medical advice is obtained
Seek medical review the same day, particularly if symptoms involve vomiting, swelling or widespread hives
If your baby is otherwise settled, breathing normally and alert, this is not an emergency, but it does require follow-up
-
Anaphylaxis is a severe, life-threatening allergic reaction that requires immediate treatment.
Call 000 immediately if your baby has:
Difficulty breathing or noisy breathing
Persistent coughing or wheezing
Swelling of the tongue or throat
Trouble swallowing or hoarse cry
Pale appearance, floppiness or collapse
Extreme drowsiness or unresponsiveness
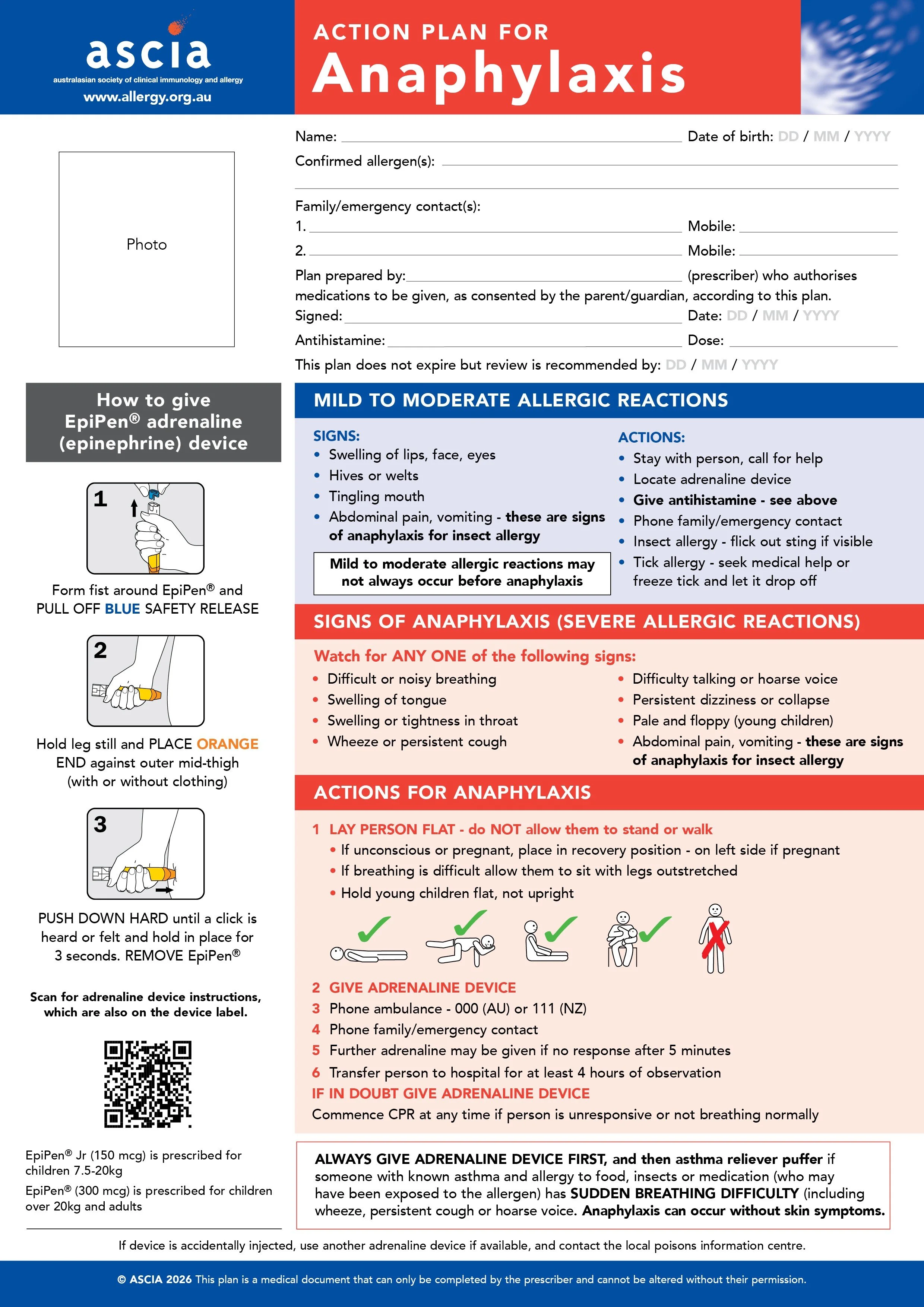
If your child has an ASCIA Action Plan and prescribed adrenaline, follow the plan and administer adrenaline immediately.
Adrenaline is the first-line treatment for anaphylaxis. Delaying treatment increases risk.
-
Write down the food and symptoms.
Avoid the food until reviewed by a health professional

FAQs
-
Having a family history of allergies (such as eczema, asthma, hay fever or food allergy) does increase the risk that a baby may develop allergies — but it does not mean they will.
Current evidence, including guidance from the Royal Children’s Hospital (RCH), shows that early introduction of common food allergens (such as egg and peanut) around 6 months of age can actually reduce the risk of developing food allergies, even in babies with a strong family history.
For most babies, allergens should be introduced one at a time, in small amounts, when they are well and during the day so they can be observed. Babies with severe eczema or a known food allergy may benefit from discussing allergen introduction with their GP or paediatrician first, but routine allergy testing is not required for most infants.
In short: a family history means extra care and observation, not avoidance — and delaying allergens may increase, rather than decrease, allergy risk.
-
Babies with eczema — particularly moderate to severe eczema — have a higher risk of developing food allergies. However, avoiding allergens is not protective. In fact, early and appropriate introduction of allergens may be especially important in these babies. If your child has eczema, ensure it is well managed and introduce allergens in safe, age-appropriate forms. If your baby has severe eczema or an existing food allergy, speak with your GP or allergist before introducing peanut, as individualised guidance may be recommended.
-
Some food allergies, such as cow’s milk, egg, wheat and soy, are commonly outgrown in early childhood. Others, including peanut, tree nut, fish and shellfish allergies, are more likely to persist into later childhood or adulthood. Regular medical follow-up is important, as tolerance can change over time and reintroduction may be possible under medical supervision.
-
Introduce allergens one at a time, starting with a very small amount earlier in the day so your baby can be observed. Always offer allergens in textures appropriate for your child’s developmental stage — for example, smooth nut pastes mixed into purée rather than whole nuts. If no reaction occurs, gradually increase the amount over subsequent exposures. Once an allergen is tolerated, include it regularly in your child’s diet to help maintain tolerance.
-
If your baby develops symptoms such as hives, swelling or vomiting after eating a new food, stop the food immediately and seek medical advice. Do not reintroduce the food until you have discussed it with a healthcare professional. If symptoms involve breathing difficulty, collapse or significant drowsiness, this may be anaphylaxis and requires immediate emergency care.
-
If your baby tolerates an allergen, it is important to keep that food in their regular diet. Removing tolerated allergens may increase the risk of developing an allergy later. Growing Plates meals are designed to support this ongoing exposure in a safe and developmentally appropriate way as your child grows.
-
Anaphylaxis is a severe, life-threatening allergic reaction that can involve the airway, breathing and circulation. Symptoms may include difficulty breathing, tongue or throat swelling, persistent coughing, wheeze, pallor, floppiness or collapse. Anaphylaxis requires urgent treatment with adrenaline and immediate medical attention. Families of children with diagnosed food allergy may be provided with an ASCIA Action Plan and adrenaline auto-injector.
-
Research shows that a baby’s immune system is most adaptable in the first year of life. Introducing common allergenic foods during this window helps the immune system learn that these foods are safe, reducing the likelihood of allergy developing later. Delaying allergen exposure without a medical reason does not prevent food allergy and may increase risk. For this reason, Australian guidelines recommend introducing allergens once babies are developmentally ready for solids (around 6 months, not before 4 months), using safe textures and small amounts, and continuing regular exposure once tolerated.
-
Growing Plates meals are prepared with careful attention to allergen identification, clear labelling and age-appropriate preparation. Our menus are designed to support early, regular exposure to allergens when safe and appropriate, while allowing families to make informed choices. We believe allergen education should feel empowering — not frightening — and that parents deserve both evidence-based guidance and practical support.
Important Information
While every effort is made to minimise cross-contact, we cannot guarantee the complete absence of allergens. For this reason, Growing Plates may not be suitable for children with diagnosed food allergies requiring strict avoidance, unless advised otherwise by a healthcare professional.
The information provided by Growing Plates is intended for general educational purposes only and does not replace personalised medical advice. Always follow your child’s ASCIA Action Plan if one has been provided, and seek immediate medical attention if an allergic reaction is suspected